Case Study: Resolving Arm Burning and Neck Tightness in a Long-Distance Runner
Sometimes “thoracic outlet syndrome” is only part of the story.
(Fascial Counterstrain Treatment – 2 Sessions)
Disclaimer: This case study is based on a real treatment session. Identifying details have been changed to protect patient confidentiality. Individual results will vary.
Background
This patient has a long history of running — 13 years of regular training, currently running 4 times per week for 5–10 km.
Their work, however, is the opposite of active: mostly desk-based and sedentary.
They also have a significant medical and injury history, including:
Abdominal surgery (no full detail given here to protect privacy)
Abdominoplasty (tummy tuck)
Several fractured toes
Multiple falls from horses and roller skates in their teens, resulting in coccyx pain so severe they could not sit in a car for long periods
In other words, this is a strong, active person whose body has also accumulated several old injuries and scars over the years.
The Main Complaint
For about six weeks before seeing me, they noticed:
Tightness in the right trapezius and neck, spreading down the arm
Burning pain in the right arm, travelling down to the wrist and little finger
Similar (but milder) burning sensations on the left side
A feeling that both hips and thoracic spine were “locked up”
Symptoms that were worse after running, with their body feeling stiff and “stuck”
They had tried yoga, but found it actually made things worse.
They described their thoracic spine as “feeling terrible” with certain movements.
First Assessment: More Than Just a Tight Neck
On examination:
Neck rotation and bending forward/backward were mostly okay
Bending the neck sideways to the left reproduced pain; to the right was better
Forward bending of the lower back was good (they could reach their toes)
Backward bending of the lower back made the thoracic spine feel tight
Neurological and mechanical testing showed:
A neurodynamic test to the right arm reproduced the burning pain down to the wrist and little finger
The left arm produced a milder version of the same burning
The first rib on the right was elevated and not moving well
The scalene muscles (small neck muscles that help you breathe and support the neck) were tight
There were multiple very tender spots and fascial restrictions around the thoracic spine
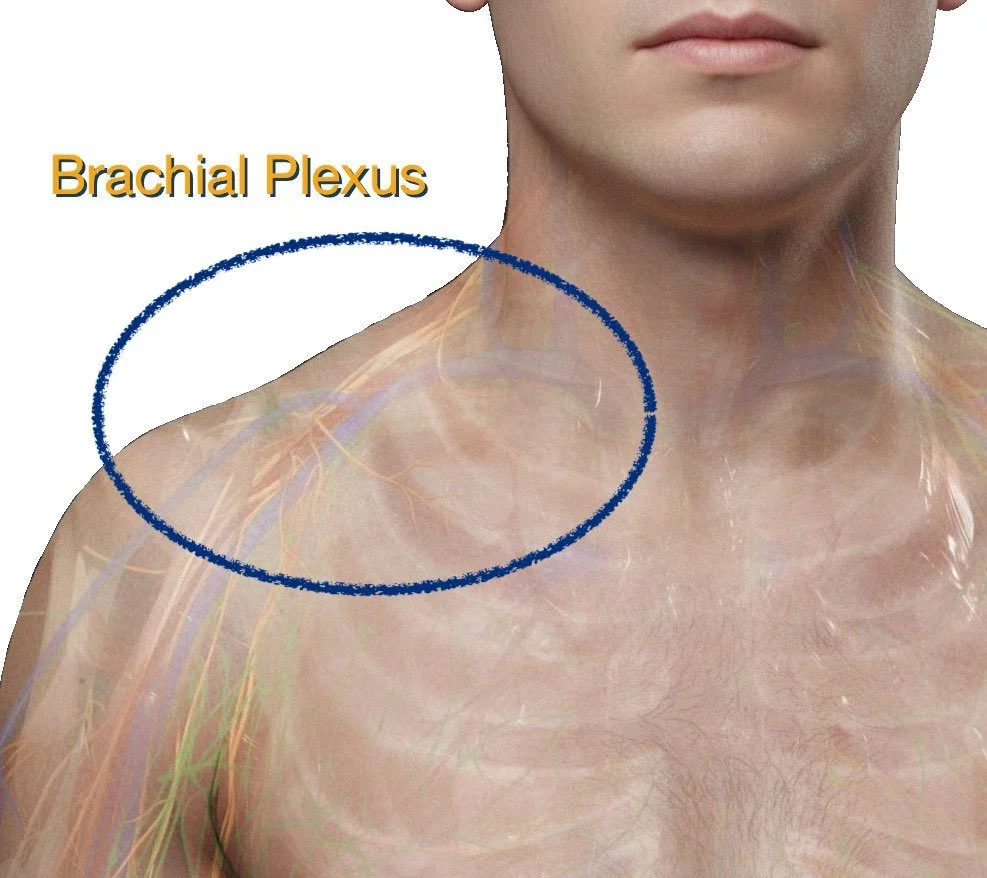
From a traditional perspective, this looks a lot like thoracic outlet syndrome – irritation of the brachial plexus (the big nerve bundle that supplies the arm) as it passes between the neck muscles and the first rib.
But I suspected there was more behind it.
Thoracic Outlet vs Nerve Root Compression
It’s worth briefly explaining the difference between two common sources of arm symptoms:
Nerve root compression (e.g. a pinched nerve at the neck):
Often causes pain, pins and needles, or numbness in a fairly predictable line down the arm, following that nerve’s dermatome.
Brachial plexus / fascial irritation (as in thoracic outlet):
Symptoms can be more patchy — burning, heaviness, odd pulling sensations that may change with shoulder, neck, or rib position.
In this case, the pattern of burning into the little finger, combined with restricted first rib movement and tight scalenes, strongly suggested brachial plexus irritation at the thoracic outlet, rather than just a “pinched nerve” in the neck.
Why Running Made It Worse
When we run, our body naturally increases its breathing demand.
That means:
The scalene muscles work harder to help lift the upper ribs
The first rib moves more with each breath
The brachial plexus, which passes between these muscles and over that rib, needs to glide and slide freely
If the scalenes are tight and the first rib is elevated or stuck, the brachial plexus can’t move properly. With each step and each breath, the nerves can become irritated — leading to burning and pulling sensations down the arm.
So yes, their symptoms were aggravated by running — but running itself was not the root problem.
Looking Deeper: Posture, Fascia, and “Why Is the Scalene Tight?”
The next important question is:
“Why are the scalene muscles tight and over-protective in the first place?”
If we only treat the tight muscle or release the nerve once, the body will often recreate the same tension pattern again and again.
Using the Fascial Counterstrain (FCS) diagnostic protocol, I found a significant restriction around the C7–T1 region — where the neck meets the upper back. This is a common stress point in people who:
Spend long hours at a desk
Develop a forward head posture
Don’t get enough regular movement breaks
Gravity constantly pulls us forward and down. Maintaining an upright head position over a sedentary workday requires strength, endurance, and good fascial glide. Without that, tissues fatigue, tighten, and begin to protect themselves.
Even in a “healthy” body, I recommend a short break every 30–45 minutes of computer work:
Stand up
Gently move your neck and shoulders
Take a few deep breaths
Have a sip of water (to hydrate the body and to create more chances to leave your seat and move to the toilet)
These small pauses help the lymphatic system clear metabolic waste, and give the fascial system a chance to “reset”.
Now, add in abdominal surgery, and the body will naturally tend to slouch to reduce fascial tension at the front. That often forces us into a rounded, flexed position, which overloads the back of the neck and upper thoracic spine even more.
We may want to sit upright, but we are constantly fighting the tight tissues at the front — and that is exhausting.
Fascial Findings: Sibson’s Fascia, Lung Apex, and Headaches
During the first session, the FCS assessment highlighted:
Restrictions in Sibson’s fascia and the fascia around the apex (top) of the lung
These fascial layers have a close relationship with the first rib, scalene muscles, and brachial plexus
Tightness there can:
Limit lung expansion at the top of the chest
Mechanically “hold onto” the brachial plexus
Contribute to arm symptoms, especially with deep breathing or running
We also found significant tension in the sub-occipital muscles at the base of the skull. The patient reported on-and-off headaches, mainly at the back of the head and worse with computer use — classic for this area.
When the sub-occipital muscles tighten, they can irritate the greater and lesser occipital nerves that pass through them, and reduce local blood flow and lymphatic drainage. The result: tension headaches and a heavy, tired head.
Using Fascial Counterstrain and gentle cranial techniques, we:
Reduced tension in the sub-occipitals
Addressed the periosteum of the upper neck vertebrae C1–3 (the fascial layer wrapping around the bone)
Released fascial restrictions in and around the first rib, scalenes, and lung apex
After that first session:
The first rib moved more freely
The scalenes felt noticeably softer
Neck movement was close to normal
They were able to go for a run the next day
Second Session: Why Did Symptoms Return?
About two weeks later, they returned for review.
They reported:
Right arm symptoms had been almost completely gone for around 10 days
They had continued running, and were mostly pain-free
The burning in the arm had returned 2–3 days before the review, without a clear trigger
Headaches were much better
On examination, there was still:
Mild restriction in the right first rib and scalene, but not as severe as the first visit
Some limitation in thoracic spine rotation in the mid-back
This told me that while the local mechanics had improved, we still hadn’t fully uncovered the root driver.
Deeper Layers: Diaphragm, Lower Back, Coccyx, Feet, and Scar Tissue
Repeating the Fascial Counterstrain diagnostic scan revealed:
Restrictions around T7–T8 and the lower rib cage, linked to the diaphragm
Restrictions in the lower back (L4–L5), sacrum, and coccyx
Tension along the plantar nerves of the feet, connecting up through the sciatic nerve to the lower back
Fascial tension related to their abdominal surgical scar (from C-section and abdominoplasty)
How could all of that relate to their arm symptoms?
Think of the fascial and nervous systems as a continuous web:
A restriction around the diaphragm can limit breathing efficiency, forcing the scalenes to work harder as accessory breathing muscles — especially during running.
Old injuries such as toe fractures can, over time, create subtle protective tension along the plantar nerves, sciatic nerve, and up into the lumbar spine.
The coccyx and sacrum, previously irritated in their teens, can hold chronic fascial tension that alters pelvic and spinal mechanics.
Abdominal scars can restrict the front of the body, influencing posture and how the spine stacks and moves.
Using FCS, we gently treated:
The diaphragm and lower rib cage
Restrictions around L4–L5, sacrum, and coccyx
The plantar nerve connections to the lower back
The abdominal scar tissue and its deeper fascial attachments
Once these deeper restrictions released:
Thoracic and lumbar mobility improved
Sacrum and coccyx moved more normally
First rib motion and scalene tone normalised again
Arm nerve tension tests (ULNT1) became normal and did not reproduce burning
The Outcome
After the second session:
The burning sensation down the right arm settled
Neck movement remained free
The first rib was moving well, and the scalenes felt soft
Headaches stayed much improved
They were able to continue running, now with a plan to support their body rather than just “push through”
Ongoing Maintenance: What We Focused On
Once the major fascial restrictions were reduced and alignment improved, the next step was simple, sustainable maintenance.
My approach is:
Exercises should be pain-free, easy to do, and realistic to maintain consistently.
For this patient, we focused on:
Gentle scalene stretches
Chin tuck exercises to encourage a more neutral neck position
Simple thoracic mobility movements
General lower limb flexibility work before and after running
Regular movement breaks during desk work
Hydration and reducing inflammatory foods to support tissue recovery and lymphatic drainage
Take-Home Message
This case is a good example of how:
Arm burning and neck tightness are not always just a “neck problem” or a local nerve issue
Thoracic outlet-type symptoms can be influenced by:
First rib mechanics
Scalene muscle tension
Fascial restrictions around the lung apex, diaphragm, and thorax
Old injuries, scars, and even foot and coccyx issues
Treating only where it hurts often isn’t enough — especially in long-standing, complex bodies
By listening carefully to the history and using a whole-body approach like Fascial Counterstrain, we can often uncover the deeper layers of restriction that are keeping symptoms alive.
If you’re a runner or spend long hours at a desk and you recognise any of these patterns — burning in the arm, neck tightness, a “locked” mid-back, or headaches from computer work — it may be worth having your whole systemassessed, not just the area that hurts.
If you’d like to explore whether this approach could be suitable for you, you’re welcome to get in touch or book an appointment.
Frequently Asked Questions
1. Can burning in my arm after running really come from my neck or ribs?
Yes, it can. Arm burning, tingling, or odd pulling sensations don’t always come from a local injury in the arm. They can be related to:
Irritation of the brachial plexus where it passes between the neck muscles and first rib
Tight scalene muscles and elevated first ribs
Fascial restrictions around the upper chest, lung apex, or diaphragm
A detailed assessment can help determine whether your arm symptoms are coming from the neck, thoracic outlet, or somewhere else along the nerve pathway.
2. What is thoracic outlet syndrome?
Thoracic outlet syndrome describes a group of conditions where the nerves and/or blood vessels supplying the arm are compressed or irritated as they pass from the neck into the upper limb.
Common features may include:
Pain, burning, or heaviness in the arm
Numbness or tingling into the hand or fingers
Symptoms that change with shoulder or neck position
In some cases, fascial restrictions and muscle tension (rather than just structural compression) can play a major role.
3. How is Fascial Counterstrain different from regular physiotherapy?
Fascial Counterstrain is a gentle, hands-on approach that:
Uses very specific tender points and diagnostic tests to locate fascial and neurovascular restrictions
Works with the body’s protective reflexes, rather than forcing through stiffness or pain
Can be applied to any fascia wrapping around muscles, nerves, blood vessels, viscera, and lymphatic structures
It can sit alongside more traditional physiotherapy approaches (such as exercise and education) and is particularly useful when symptoms seem to involve multiple regions or systems, not just one joint or muscle.
4. Do I need to stop running if I have these symptoms?
Not always. In this case, the patient was able to continue running while treatment addressed the underlying restrictions.
In general, whether you need to modify or pause running depends on:
The severity of your symptoms
Whether running is clearly aggravating the condition
How your body responds to early treatment
Often, a tailored plan will include:
Short-term modifications (distance, pace, terrain)
Specific exercises to support your neck, thoracic spine, and lower limbs
A gradual return or progression as symptoms settle
5. When should I seek help for arm burning or neck tightness?
You should seek professional assessment if:
Arm burning, tingling, or numbness persists for more than a few days
Symptoms are worsening, or spreading into the hand
You notice weakness, loss of grip strength, or difficulty with fine hand tasks
Symptoms interfere with your work, running, or sleep
Early assessment can help identify contributing factors and reduce the chance of the problem becoming long-standing.
This article is for general information only and does not replace individual medical or physiotherapy advice. If you have similar symptoms, please seek a personalised assessment from a qualified health professional.